Diabetes Moonshot: Addressing a Growing Health Challenge
In the Netherlands, approximately 1.2 million people are diagnosed with type 1 or type 2 diabetes. That means one in every fourteen individuals will face this diagnosis at some point in their lives. Of these, 10% are attributed to type 1 diabetes. (Source: Dutch Diabetes Research Foundation - Diabetes in Figures)
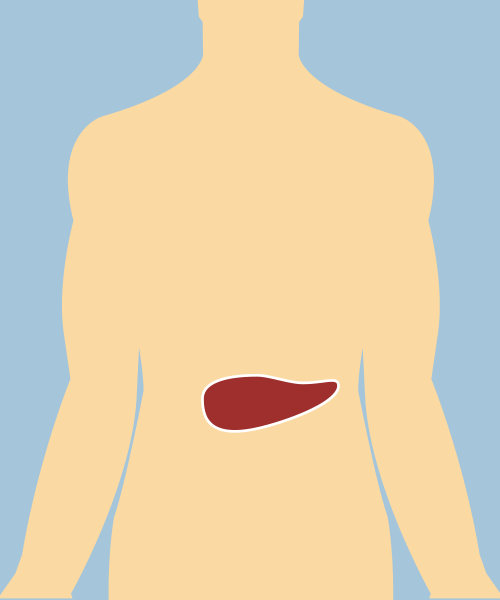
In individuals with type 1 diabetes, the body’s immune system destroys insulin-producing beta cells in the pancreas. Insulin is a crucial hormone that enables cells to absorb glucose (sugar), providing the energy needed for proper bodily function. It also plays a key role in regulating blood glucose levels, ensuring they remain stable without significant fluctuations.
RegMed XB’s Diabetes Moonshot: A Path Toward a Better Future
RegMed XB’s Diabetes Moonshot aims to develop a regenerative medicine solution for type I diabetes: a combination therapy that combines insulin-producing cells and a biomaterial implant.
Since those with type 1 diabetes produce little to no insulin, they must constantly monitor their blood glucose levels. By accounting for factors like meals and physical activity, they calculate and administer the appropriate insulin doses. Unfortunately, replicating the body’s natural insulin production is very difficult, often leading to considerable glucose fluctuations.
Prolonged high blood glucose levels increase the risk of severe complications like blindness, heart and blood vessel damage, nerve degeneration, and kidney failure. Conversely, dangerously low blood glucose levels can cause confusion, drowsiness, or even coma. Managing diabetes can take a significant toll on both the physical and mental well-being of patients, often lowering their quality of life.
Achievements and future roadmap for the Diabetes Moonshots
In recent years, progress has been made in developing insulin-producing islets. A new purification method optimizes the quality and potential of these beta cell islets.
Looking ahead, one of the main challenges will be scaling up the transformation of stem cells into insulin-producing cells, needed to ensure a steady and sufficient supply of islets for future research and treatments.
The biomaterial implant is undergoing extensive testing. A protective open structure has been chosen, but several aspects must be validated before it can be used in clinical trials. Safety and robustness of the implant is critical to ensure its quality, and longevity.
Additionally, ongoing experiments are testing the function of the cells and assessing the biomaterial's compatibility and tolerance within the body.
Finally, one potential high risk for clinical use of the implant is a general immune reaction against the implant, so careful testing is required. Although the product is not near clinical use yet, step-by-step we are moving in that direction.
